Water is an essential component of body composition, and proper hydration is essential for maintaining overall health and well-being. Seniors are particularly challenged by hydration problems due to a combination of factors, including:
- Decreased sense of thirst response related to age and/or medications
- Avoidance of liquids, sometimes in effort to avoid incontinent episodes
- Difficulty accessing or consuming beverages independently due to decreased mobility, strength and dexterity
- Symptoms of dysphagia (difficulty with swallowing) related to neurological medical conditions, including multiple sclerosis, Parkinson’s disease and stroke
- Cognitive impairments; simply forgetting to drink fluids- which could lead to dehydration
- Increased isolation due to infection control policies
You may be asking “how much water should an elderly person drink a day?” and “how can you encourage the elderly to drink more water?” The answer varies, but when summer temps start to soar, keeping seniors properly hydrated gets even harder. With that in mind, here are five easy ways to help promote hydration for seniors in your community.
1. Keep Water at Hand in Residents’ Rooms
Insulated mugs are a great way to keep water refreshingly cold and promote hydration in seniors. When caregivers come around to check in on residents or deliver medications, they can also refill mugs. It’s also an opportunity to make sure drinks are within reach of residents and to remind them to drink.
It’s important to remember that cold water is not always a preference. Room-temperature or water with no ice is sometimes preferred, as it may be easier to swallow, limits constriction during swallowing and reduces the feeling of being “chilled” that many older, frail adults experience.
Clear mugs allow both residents and caregivers to easily see how much liquid has been consumed and how much remains. Some styles have graduated markings for easy intake tracking. From a dignity standpoint, be sure to offer cups and glasses that allow residents to independently serve themselves without assistance.
Another approach to foster hydration in the elderly is to have two mugs of different colors for each resident – one to be consumed each morning and another to finish over the afternoon. This may increase seniors’ water intake throughout the day.

2. Set Up Beverage Stations in Common Areas
Make beverages equally accessible and convenient outside resident rooms in shared spaces, like lobbies or activity areas. This visibility may encourage residents to drink more during the day.
Consider setting up a refrigerated grab-and-go beverage station in high-traffic areas. Or use mobile beverage carts to take hydration on the move, with a staff member proactively offering drinks to residents as they pass through the building.
Stock your stations with a variety of healthy hydration drinks to cater to individual tastes and preferences. Fruit juices, iced tea and even milk are good healthy hydration alternatives that may appeal to residents who don’t enjoy plain water.
Don’t forget to include the following convenience items:
- Straws may make drinking easier for some residents
- Paper napkins keep things tidy by capturing condensation
- Sweeteners complement coffee and tea
- An ice scoop or tongs help ensure sanitary service of ice cubes

3. Tempt Residents with High-Hydration Snacks
To prevent dehydration, integrate mouth-watering snacks into your Senior Living meal plan this summer. Many fruits are at their best over the summer months and will give an extra boost of color and flavor to menus. Melon has a particularly high water content, but berries, citrus fruits, stone fruits and tropical fruits are all juicy options to explore.
Outside of mealtime, snacks such as Jell-O cups and applesauce cups will feel right at home on a hydration station. And other tasty treats, like sherbet or popsicles, could replace cakes and cookies on your summer dessert menu as hydrating foods for seniors.
Certain foods and snacks can help better absorb water. Fibrous foods retain water and slowly dissolve. Slow absorption can help seniors stay better hydrated for longer time periods. High-fiber snacks to infuse into senior dining include apples, berries, citrus fruits and pears, as well as barley, oatmeal, beans and nuts.

4. Turn Hydration into a Social Event
Everyone loves an ice cream social! Consider offering soft-serve since it has a higher water content. Include an assortment of toppings and you’ve got a ready-made sundae bar.
Happy hour events are another fun way to bring residents together while sneaking in extra hydration. But beware – alcohol has a diuretic effect, so it won’t help at all with hydration. Try serving non-alcoholic beer, margaritas and sparkling fruit juices to conjure up a social atmosphere while advancing hydration goals.
To encourage seniors to stay hydrated, try hosting social events in alternative spaces. Hydration socials can occur in hallways, outdoor spaces or even be combined with room delivery service or a virtual “happy hour” style event.
5. Hot Beverages or Not?
Hot beverages may not be the first thing you think of when it comes to summer hydration, but don’t dismiss them too quickly. It’s true that, like alcohol, caffeine has a diuretic effect. While decaf options will make sense for some, other residents may not need to avoid caffeine entirely. Insulated disposable cups and ceramic mugs are great for keeping hot drinks the perfect temperature.
Evidence shows that seniors who are already regular coffee or tea drinkers will maintain a more optimal fluid balance when continuing with moderate caffeine consumption, rather than by refraining.1
What does “moderate” consumption look like? That’s about 250 to 300mg of caffeine per day, or the equivalent of 2 to 3 cups of coffee, or 5 to 8 cups of tea.
What is the Recommended Fluid Intake for Seniors?
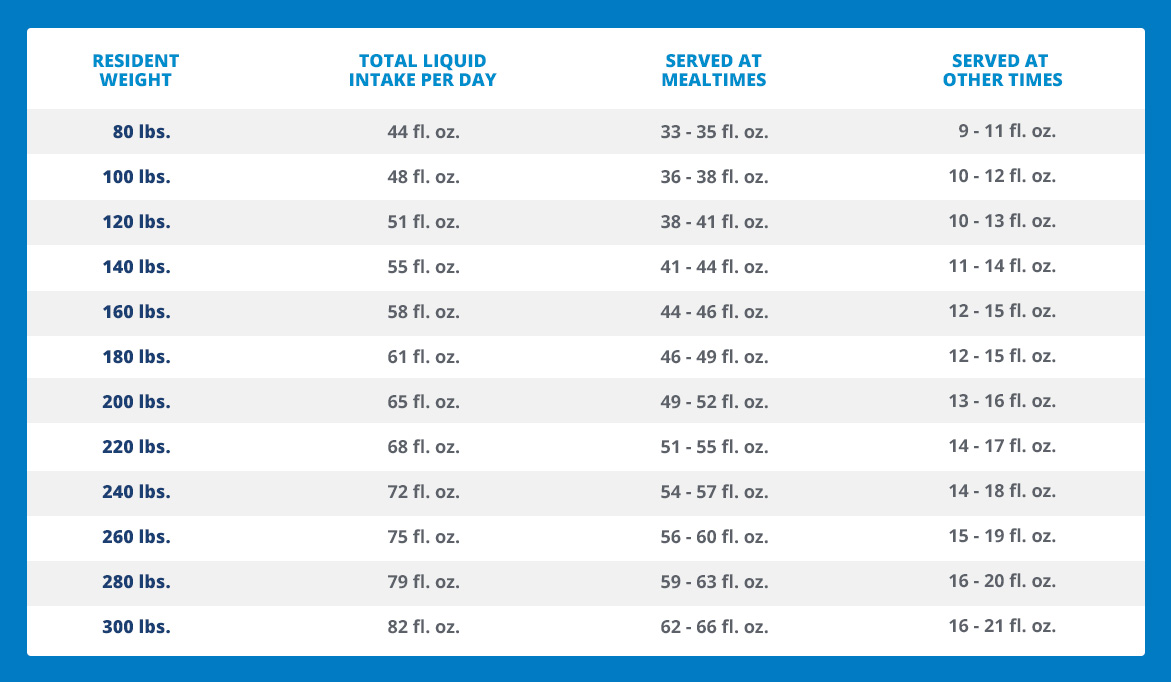
Use this fluid intake chart for seniors to approximate total liquid intake goals based on body weight. A handy rule of thumb is to serve 75% to 80% of total fluids during mealtimes, and 20% to 25% of total fluids outside of mealtime hours.
1. Boltz, Capezuti, Fulmer and Zwicker (Editors). Evidence-Based Geriatric Nursing Protocols for Best Practice. Fourth Edition. Maughan & Griffin, 2003.




